Systemic medical discrimation and abuse, pt. 1: Public scandals
I have been meaning to write about this before now, but have held off because it’s very triggering with my own medical PTSD, and because my own regular pain levels lately have been making it hard to do much writing. But, it’s an important subject, and more people need to be talking about it. (I’m feeling kind of overwhelmed, and may not do the best job of this, BTW.)
Readers outside the UK may or may not have heard of the Mid Staffordshire hospital scandal which is (thankfully) continuing to get a good bit of attention here. In short:
An estimated 400-1,200 patients died as a result of poor care over the 50 months between January 2005 and March 2009 at Stafford hospital, a small district general hospital in Staffordshire. The report being published on 6 February 2013 of the public inquiry chaired by Robert Francis QC will be the fifth official report into the scandal since 2009, and Francis’s second into the hospital’s failings.
The often horrifying evidence that has emerged means “Mid Staffs” has become a byword for NHS care at its most negligent. It is often described as the worst hospital care scandal of recent times. In 2009 Sir Ian Kennedy, the chairman of the Healthcare Commission, the regulator of NHS care standards at the time, said it was the most shocking scandal he had investigated…
Francis’s report into care at Stafford hospital in February 2010, based on evidence from over 900 patients and families, was scathing. “I heard so many stories of shocking care,” he said. “They were people who entered Stafford hospital and rightly expected to be well cared for and treated. Instead, many suffered horrific experiences that will haunt them and their loved ones for the rest of their lives.”
Francis cited a litany of failings in the care of patients. “For many patients the most basic elements of care were neglected,” he said. Some patients needing pain relief either got it late or not at all. Others were left unwashed for up to a month. “Food and drinks were left out of the reach of patients and many were forced to rely on family members for help with feeding.” Too many patients were sent home before they were ready to go, and ended up back in hospital soon afterwards. “The standards of hygiene were at times awful, with families forced to remove used bandages and dressings from public areas and clean toilets themselves for fear of catching infections.” Patients’ calls for help to use the toilet were ignored, with the result that they were left in soiled sheeting or sitting on commodes for hours “often feeling ashamed and afraid”. Misdiagnosis was common…
(That is indeed a very brief summary. It’s really awful stuff, chock full of systemic problems with accountability and higher handling of complaints during that time period. Here’s a brief timeline. Serious problems were evident from at least 2002 on, and nobody did anything about the problem.)
Five other hospital trusts, mostly running multiple hospitals each, are under investigation for similar problems. Our rather horrible local hospital (there were recently only two hospitals patients would recommend less in the entire country), along with one other, also has nine cases being brought against it now for human rights violations. Why?
The cases are being prepared by specialist lawyer Emma Jones of Leigh Day and Co. on grounds of negligence and poor care standards. Two have so far reached the High Court.
Ms Jones told the Romford Recorder she started receiving calls from families after the publication of a damning report by the Care Quality Commission (CQC) into the Rom Valley Way hospital last year.
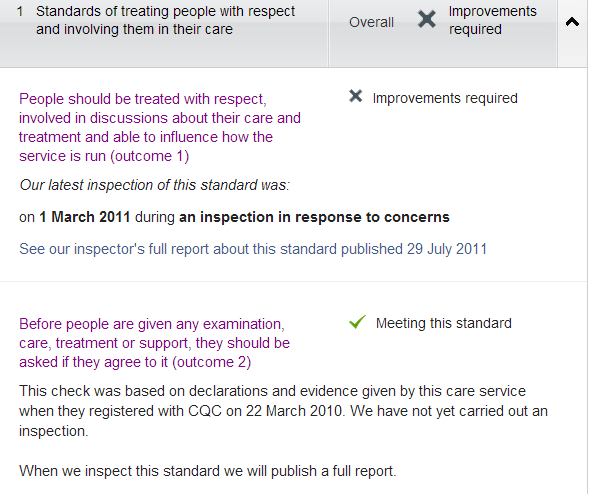
Update on CQC investigation report June 2012 – Queen’s Hospital. (PDF) There have been serious problems officially recorded, including bullying and harassment of people trying to make complaints (sound familiar?), for years and years. I will include a screenshot from the CQC’s listing for the hospital:
From the same organization earlier this year: Regulator finds that A&E department at Queen’s Hospital, Romford, is still failing to protect the safety and welfare of people. That is their own headline. Which sounds an awful lot like “caring for people safely and protecting them from harm”, the only passing-level standard listed above.
Also, expanding one of the (overall unsatisfactory) items:
They are apparently defaulting to “Meeting this standard” before actually investigating, based on “declarations and evidence given by this care service”. Like the organization is going to say, “No, we don’t give a damn about informed consent, or any consent whatsoever!” This leads to some concerns about the standards for some other ratings under the CQC.
Besides the fact that this is our local hospital, and I have felt like it was wiser to actively avoid seeking treatment there when I have really needed it on multiple occasions, this is an excellent example of the lack of accountability and action over known problems. What are they going to do, close down an already absurdly busy teaching hospital when it doesn’t meet basic standards? No. They are going to let it continue operating in very bad ways, while anyone who tries to complain about the problems gets brushed off and abused, including people working within the NHS (tot he point of gagging clauses).
This is not an unusual problem, and it is hardly limited to the NHS (though the huge bureacratic setup does not help). I could certainly tell some stories from a number of hospitals in the US. (More on that later, with an ongoing situation happening right now.) The institution is much more important than the actual humans which compose it, not to mention the ones relying on it for lifesaving care.
I’ve gone more into the bigger institutional picture here than intended, partly because the further down you go, the more infuriating and depressing it gets.
What keeps getting the blame for the deaths and abuses here? Serious understaffing. No doubt that does create problems, but just the fact of overworked staff does not adequately explain why certain groups of people keep getting neglected, abused, and allowed to die.
This keeps getting hinted at.
“A chronic shortage of staff, particularly nursing staff, was largely responsible for the substandard care,” Francis found in his first report.
In addition, morale was low and “while many staff did their best in difficult circumstances, others showed a disturbing lack of compassion towards their patients”, he added. “Staff who spoke out felt ignored and there is strong evidence that many were deterred from doing so through fear and bullying.”
He laid much of the blame on the trust’s ruling board. The action they took to investigate and resolve concerns “was inadequate and lacked an appropriate sense of urgency”. Its members also “chose to rely on apparently favourable performance reports by outside bodies, such as the Healthcare Commission, rather than effective internal assessment and feedback from staff and patients”. He was particularly critical of the trust’s failure to take patients’ complaints seriously enough. #
(I left that last paragraph in, just because.)
People in Stafford are rightly upset and angry, and the report sets out some examples that are very hard to read. I would never want a member of my family to suffer the indignity, pain and fear that some patients at Stafford endured. At the inquiry, relatives gave damning evidence of the unacceptable care their loved ones suffered. I was horrified to read that they described wards as resembling a “war zone”, with “buzzers not being answered, privacy and dignity ignored and patients receiving little or no help with food and drink”.
In 1859, Florence Nightingale said that “the very first requirement in a hospital is that it should do the sick no harm”. And yet, here in the 21st century, we are facing the uncomfortable truth that patients suffered at the hands of nurses.
What makes me most upset is that patients in need of care were let down by staff who squandered the trust the public has traditionally put in nurses, the caring profession. The reality is that there are some nurses who do not have the capacity to be compassionate and truly care, despite training and support. They have no place in the NHS. We only want nurses who come to work to make a difference for their patients and are prepared to take personal responsibility for individuals in their care. They must be supported by good leaders, who understand the pressures and challenges of being a nurse or midwife, but first and foremost they must want to care for their patients. There is no room in the nursing and midwifery professions for people who don’t have empathy with their patients. As Robert Francis points out, those patients are increasingly older people who require specialist nursing skills and commitment from their nurses. #
I have, however, been disturbed at not that much attention going to the fact that it is certain groups of people who are at the most risk of medical abuse and neglect, perhaps amplified by not enough nurses available. The main people I have seen talking about this, at all, are their family members.
Among those making claims are the family of Ronald Roast, of Rainham.
Mr Roast was admitted to Queen’s in 2011 after suffering a series of heart attacks. He had advanced lung cancer and died of the illness in St Francis Hospice, Havering-atte-Bower, the day after he was discharged. He was 69.
Daughter Maria Lloyd, of Cricklade Avenue, Harold Hill, alleged her father hadn’t been fed properly while he was at Queen’s, and had gone 12 hours without a drip.
“It felt like the fact he was dying meant they didn’t really have much time for him,” said Maria, 47.
“He was just hauled about. They didn’t even check he was eating properly or going to the toilet. #
_
Her daughter, Maria Lloyd, claimed that because he was dying, medical staff had simply appeared not to care.
“It was just awful,” she said. “The nurses who were changing him left the curtains open and hadn’t covered him up properly.
“There was just no dignity. He was dying but you can’t treat people like that. At the end of the day if you go into hospital you expect to be treated with respect and dignity. I thought we had gone back to the 1800s.”
Robin Tilbury’s mother Patricia, 85, died at Eastbourne District General in November 2011. She had cancer and had been admitted with malnutrition.
Mr Tilbury said he believed she had been denied vital nutrition supplements and had not been monitored “in any way”.
Emma Jones, a human rights lawyer with solicitors Leigh Day & Co, said: “We are talking about people who have been left without hydration, who haven’t been given food, whose medication has been missed. Many care issues.
“We are talking about people who are often elderly, they are vulnerable and I can understand completely why relatives of their loved ones would believe that such poor treatment and care might have contributed to their death. #
_
A criminal investigation has begun into the death of a diabetic woman at scandal-hit Stafford Hospital, the Health and Safety Executive (HSE) has said.
Gillian Astbury died after slipping into a diabetic coma at the hospital in 2007. An inquest in 2010 found that the failure to administer insulin to the 66-year-old patient amounted to a gross failure to provide basic care…
Astbury, from Hednesford, Staffordshire, died on 11 April 2007 while being treated for fractures to her arm and pelvis.
Jurors at the September 2010 inquest found that a contributory factor in her death was a systemic failure to provide adequate nursing facilities and low staffing levels.
The inquest heard that Astbury’s blood sugar levels were not properly monitored and insulin was not administered on the day before her death, despite being prescribed by doctors.
A police investigation was launched after her death, but the Crown Prosecution Service ruled that there was insufficient evidence to bring charges. #
_
Although 41 nurses have been referred to the NMC since the first of two reports into the hospital by Robert Francis QC in early 2010, none has so far been disciplined in any way. Of those, action against 31 was considered but discontinued due to what the regulator said was a lack of evidence.
It has begun disciplinary proceedings against Reni Biju, a nurse who is accused of misconduct involving four patients in separate incidents during 2009-10, long after the first concerns emerged about the hospital. She is accused of walking away from a female patient who asked her to pass her a hearing aid and then, when the same patient pressed her call bell because she needed help to visit the toilet, cancelling the call bell and walking away and, soon after, giving the patient her walking frame and letting her go to the toilet unaided. Biju “showed no interest in Patient D’s safety and wellbeing”, the NMC claims
It will also next week begin a fitness to practice hearing into claims that Bonka Kostova, a midwife working as a healthcare support worker, gave inadequate care to a patient who had Alzheimer’s disease. The NMC claims that she “pushed Patient A back into his chair when he stood up; used your body weight to push Patient A into the bathroom [and] onto the toilet; pulled Patient A out of the bathroom in a state of undress; raised your voice and/or shouted at Patient A 1) ‘I hate you’ or words to that effect [and] 2) ‘You are no longer a human being but an animal’, or words to that effect.”
Katherine Murphy, chief executive of the Patients Association, said: “The NMC and the GMC have a duty to act where poor practice and a lack of care, compassion or dignity from healthcare professionals is identified. Tragically this did not happen for those treated so appalling at Stafford Hospital.” #
Bolding added on that last quote. These things happened at different hospitals, but they all sound very similar. And what kind of evidence can you provide of that kind of treatment, without the patient recording it? Is it even likely to be taken seriously if they are able to do that? Who is considered credible is also a problem here, with the power dynamics. This is another example of why I keep talking about a wider abuse culture, based on differential respect.
Just being overworked is not an adequate explanation, much less excuse, for placing such a low priority on providing very basic, often lifesaving care, to certain groups of people. Also placing low priority on staffing for, say, geriatric wards where they know they are going to need to provide more care than they would with younger, more able-bodied people (like, erm, making sure people can eat and drink) is part and parcel of the same problem. Deciding that certain kinds of people don’t deserve what limited resources are available is a very different matter. I am afraid that this is considered normal and inevitable enough not to even warrant much comment, which is disturbing in its own way.
Understaffing does not, in itself, create depraved indifference, and “callous disregard for human life” is exactly the underlying problem here. Deciding that certain people do not deserve basic respect and dignity is the problem.
While the focus here has been on older people, I am sure that disabled people have also been getting the short end of the stick here, thanks to other people’s ideas about their worth, “usefulness” and “quality of life”. More on that, in the second part. This post has grown, and I don’t want to banish my other major focus here to the bottom of a long single post; it’s too important.




I think the above confirms, if anything, the notion that ‘there is no such things as rights, human or otherwise; rather, there are privileges which must be earned (on an ongoing basis, no less)’.
Furthermore, not everyone starts from the same place – and where one starts from is determined more or less exclusively by those who have power over one. As such, all relations are ultimately Narcissistic, with the greater seeing the lesser as ‘an objectified tool’. When such a tool is no longer useful, it is simply discarded.
Dark, yes – but accurate.
More importantly, this ‘way of being’ is evil. It must be stopped, and I wish I knew how to do so.